 The site of a beating heart glistening and pumping is like no other site I have ever seen. The heart is simply amazing. It's more than just a four-chambered pump; it is well-designed machine that keeps our blood flowing to our muscles and lungs, ensuring we receive oxygen and nutrients to sustain ourselves.
The site of a beating heart glistening and pumping is like no other site I have ever seen. The heart is simply amazing. It's more than just a four-chambered pump; it is well-designed machine that keeps our blood flowing to our muscles and lungs, ensuring we receive oxygen and nutrients to sustain ourselves.Friday, November 30, 2007
The Heart Exposed
 The site of a beating heart glistening and pumping is like no other site I have ever seen. The heart is simply amazing. It's more than just a four-chambered pump; it is well-designed machine that keeps our blood flowing to our muscles and lungs, ensuring we receive oxygen and nutrients to sustain ourselves.
The site of a beating heart glistening and pumping is like no other site I have ever seen. The heart is simply amazing. It's more than just a four-chambered pump; it is well-designed machine that keeps our blood flowing to our muscles and lungs, ensuring we receive oxygen and nutrients to sustain ourselves.Wednesday, November 28, 2007
The Special Man
Normally, Wednesday lunch is reserved for U-TEACH, an elective that takes us through the prenatal care and the birthing process. The scheduled In-Vitro Fertilization lecture was replaced with a Men in Women's Health panel, featuring an intern in OB/GYN in his first year of training and a faculty member that has spent the last 17 years at UCSF in OB/GYN.
Some of the issues that were discussed included the challenges, rewards, societal taboo associated with being a male in a field that focuses on women's health, and the downsides to being a male in the field.
One of the biggest challenges occurs when female patients will only see female providers (I place myself in this group). In that case, there is not much to do aside for apologizing or offering an female provider (if one is on hand).
Both panelists expressed a deep interest in their fields. They agreed that it is difficult to empathize with woman, having not experienced the contractions of labor or the pain of menstruation. But at the same time, they feel listening and paying attention to their patients can help make up for this deficit.
Some of the more interesting discussions revolved around what it's like for a male OB/GYN to focus his attention "down there" all the time and those conversations with significant others or friends that emerge, or the awkward silence that comes after telling others what one does for a living.
Also, panelists touched on the role of becoming sensitized to women. I suppose if you are a male and you see female patients all day, there is a possibility that the novelty of the female body wears off.
But that's where you learn to keep professional life separate from clinical life.
Overall, an interesting panel. Hopefully, the panelists were able to reach out to this "special man."
Tuesday, November 27, 2007
On a Scale of 1 to 10
 On a scale of 1 to 10, how would you describe your pain? This is a question that gets to the heart of assessing the severity of pain. And yet, how accurately can we quantify pain given everyone has a different pain threshold?
On a scale of 1 to 10, how would you describe your pain? This is a question that gets to the heart of assessing the severity of pain. And yet, how accurately can we quantify pain given everyone has a different pain threshold?Pain perception varies from person to person, and can be affected by different conditions.
Patients with fibromyalgia experience a lower threshold of pain (they are more sensitive). There are certain trigger points where pain is most pronounced; patients will experience muscle, joint pain, and fatigue.
Today in preceptorship, we confronted the issue of pain management and fibromyalgia.
"You do not hunt a rabbit with a cannon," said Dr. D.
Dr. D extended this analogy to pain management; you do not overuse opiates or pain killers when managing pain.
Dr. D has a good point--but I wonder about how to adequately help patients in pain without making them dependent on medication. And we must remember pain sensation is subjective, with a different scale for each individual.
Saturday, November 24, 2007
Thursday, November 22, 2007
Giving Thanks!
 If I had to choose a favorite Holiday, it would definitely be Thanksgiving! This holiday is shrouded in a great deal of historical controversy and I will not delve into any of that. But I appreciate the simplicity and beauty that comes from two of my favorite things: food, family, and giving thanks (OK, that is three things).
If I had to choose a favorite Holiday, it would definitely be Thanksgiving! This holiday is shrouded in a great deal of historical controversy and I will not delve into any of that. But I appreciate the simplicity and beauty that comes from two of my favorite things: food, family, and giving thanks (OK, that is three things).Wednesday, November 21, 2007
Break!
 It's break time! From noon yesterday until Monday morning at 8 AM, we have our first official break. Thanksgiving!
It's break time! From noon yesterday until Monday morning at 8 AM, we have our first official break. Thanksgiving!Before making the journey back home, I spent my afternoon at Jane's prenatal appointment. The waiting room was filled with expecting moms and the temperature was as cold as ever. It's the 25th week. Jane is doing well; her mother and father will be visiting soon. She is anxious to see her family.
The babies are moving a lot and being monitored very closely on ultrasound. On the black screen, we could make out the little hands of Baby A (the boy), who was either punching or attempting to wave. We could see Baby B's (the girl) heart pounding. On average, the babies should be kicking at least 5 times an hour.
Jane will also have her blood checked for gestational diabetes, a condition that some pregnant woman develop during pregnancy. According to the American Diabetes Association, approximately 4% of pregnant woman will develop this condition, which can result in hyperglycemia (high blood sugar).
Normally, sugar is broken down by a insulin, a hormone secreted by the pancreas. But in pregnancy, the growing placenta secretes hormones that prevent insulin from working. As a result, higher blood sugar pools in the blood, which move into the placenta and can cause birth defects and complications in pregnancy.
For more information on Gestational Diabetes: http://www.diabetes.org/gestational-diabetes.jsp
Image: "Gestational Diabetes." http://www.pennhealth.com/health_info/diabetes2/images/19724.jpg
Monday, November 19, 2007
The Power of Touch
 Come on. Admit it. You are afraid of something. Even Superman was not invincible--there was krypnonite.
Come on. Admit it. You are afraid of something. Even Superman was not invincible--there was krypnonite.Sunday, November 18, 2007
I can't get the Heart off my Mind
 Just thought I'd share what's going through my mind...it's more of an obsession with knowing the heart with an exam in less than 24 hrs...
Just thought I'd share what's going through my mind...it's more of an obsession with knowing the heart with an exam in less than 24 hrs...Image: http://library.med.utah.edu/kw/pharm/hyper_heart1.html
Saturday, November 17, 2007
Lub Dub S3
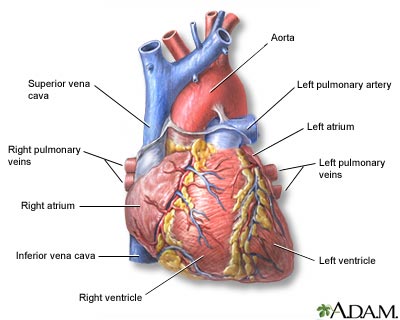 The real heart looks something like this. But the veins are not color coded (there is no blue; just shades of red).
The real heart looks something like this. But the veins are not color coded (there is no blue; just shades of red).I can not get the heart out of my mind. I know the heart is the universal sign of love, but it has occupied my brain for other reasons. Our cardiovascular midterm is on Monday.
Thursday, November 15, 2007
When the War Comes Home
 Consider this ethical question: would you be willing to kill one violent/evil individual at the expense of 3 innocent individuals? If no, do you think it's justifiable to send someone in your stead to take care of this business?
Consider this ethical question: would you be willing to kill one violent/evil individual at the expense of 3 innocent individuals? If no, do you think it's justifiable to send someone in your stead to take care of this business?Wednesday, November 14, 2007
Dinner with Dean
 Last night was a Thanksgiving preview. Our college dinner featured the Dean of UCSF and a harvest theme, complete with decorative squash, pumpkins, turkey, asparagus, potatoes, and white table clothes.
Last night was a Thanksgiving preview. Our college dinner featured the Dean of UCSF and a harvest theme, complete with decorative squash, pumpkins, turkey, asparagus, potatoes, and white table clothes.http://www.lakejunaluska.com/uploadedImages/Lake_Junaluska/Packages/thanksgiving.jpg
Sunday, November 11, 2007
Christmas, Cider, and Clinic Visit
 It is already Christmas. Well, that is, if you happen to be at Starbucks. While I was standing in line beside some of my dearest undergraduate friends, debating whether to order the usual overpriced venti chai tea latte or the seasonal peppermint mocha or the caramel spiced apple cider, Dr. Y asked me if I was interested in getting any dessert.
It is already Christmas. Well, that is, if you happen to be at Starbucks. While I was standing in line beside some of my dearest undergraduate friends, debating whether to order the usual overpriced venti chai tea latte or the seasonal peppermint mocha or the caramel spiced apple cider, Dr. Y asked me if I was interested in getting any dessert. The clear glass box housed big chocolate chunk cookies, thick slices of pound cake, cheesy bagels, nutty brownies, and rice-krispy treats. All so tantalizing and seductive.
I saw two patients and in the course of the day, I learned about everything from hypertension risk factors to ace inhibitors to syphilis to diabetes management to composing a SOAP note to viral rash presentation. I also injected my first flu shot and counseled my first patient about the numbers written on his lab tests.
Managing chronic conditions, such as diabetes and hyptertension, can be challenging. To help patients, who are at a higher risk of developing these metabolic syndromes, we encourage a healthy diet and excercise.
When I recommended regular excercise to a patient, he asked me if "sex was a type of excercise." I guess it is. I recommened a more traditional source of cardiovascular activity, like biking or walking. We'll see how that goes...
Discussing diet and excercise with patients, always make me more conscious of my diet and fitness level, a constant reinforcement of eating 5-vegetables a day, excercising and giving up the goodness that is cookies and sweets.
There are lots of firsts. And my first return to Shifa as medical student is truly memorable. I still remember the good old clinic days, when I would see the first and second year medical students in their short white coats and stethoscopes taking care of a patient, with so much knowledge and skill, while talking to the physician in a completely different language that was filled with big medical words. Now I am one of those medical students in a short white coat with my red stethoscope.
It is hard to believe that I am now in the position. I feel so lucky to be able to return and provide my services to the patients, who contributed to my passion for medicine. And being reunited with the undergraduate volunteers I worked directly with during my time at Shifa is like the cream on top of the spiced apple cider I ordered at Starbucks.
The undergraduates are the nuts and bolts of the clinic; without them- there would be no clinic. When I was a volunteer and Dr. Y, the director and my mentor, would say this to me, I did not fully understand this meaning until I returned on the other side. I will remain a Shifa volunteer, and I hope I can return to serve future patients in clinic and work alongside such dedicated volunteers.
Happy early Christmas to anyone visiting Starbucks. And I hope you will think twice about grabbing something sweet (such as the big choclate chunk cookie, my personal favorite) from behind the glass window. Well if you do go for it, just excercise the calories off (in any activity you please :)
***
For more information about Shifa Clinic (Mission, Volunteering, Donating, etc): http://shifaclinic.org/
Images: "Caramel Apple Cider." (it's too sweet for my preference). http://www.kvue.com/sharedcontent/dws/img/11-05/1122brllstarbucks.jpg
Saturday, November 10, 2007
Decisions
And to further complicate this, how about being given only a week to make this decision?
No parent should have to make this decision. But this is a reality when dealing with possible complications of a pregnancy.
The developing baby relies on the amniotic fluid for protection and proper development of muscles and organs. When we think of a baby swimming in the womb, the amniotic fluid serves as the medium of movement.
By the second trimester, the baby will begin to swallow the amniotic fluid and breathe. The mother provides the fluid up to 20 weeks of development and later the baby's urine will add to the fluid. For proper development, there must enough amniotic fluid.
In a condition know as Oligohydramnios, the placenta has low amniotic fluid, which is problematic for the developing fetus. Because of the low amniotic fluid a number of outcomes are possible: the developing fetus may not make it to term (and die in utero), experience delayed development in the organs, or may be born normally.
When the ultrasound reveals findings indicative of Oligohydramnios, the Obstetrician and Neonatal Specialist must inform the parents about their options. And one option is to terminate the baby in utero with an injection of potassium chloride into the heart to stop future contractions.
This option is complicated in the case of a twin pregnancy, when there is another developing fetus. Injecting into the womb poses the risk of infection to both fetuses, as well as premature delivery. Also, the terminated fetus would not be delivered; it would remain in the womb. So, the mother will be continue to carry both fetuses: one that is viable and one that has died.
It is hard enough to make such a decision. But how about carrying a dead fetus for a few months?
There is no way to know what is the right option or decision. The mother and her family will need to carefully consider each option and the impact it will have on their lives. It's difficult to even fathom being placed in such a situation.
And yet, this is what Jane and I were discussing at her last prenatal appointment.
Wednesday, November 7, 2007
A Day in the Life of a Medical Student- Uncovered
 The title says it all- the Class of 2010's class play basically uncovered everything. Cole Hall, our normal lecture hall, was transformed into a stage and was packed to the brim. The annual play was organized by second year medical students and featured faculty members and students in a series of skits, movies, dances, songs, off-color jokes, and innuendo.
The title says it all- the Class of 2010's class play basically uncovered everything. Cole Hall, our normal lecture hall, was transformed into a stage and was packed to the brim. The annual play was organized by second year medical students and featured faculty members and students in a series of skits, movies, dances, songs, off-color jokes, and innuendo.I was there as an audience member and photographer for Synapse.
 The play was absolutely hilarious. Probably because, it's nerdy humor that only we would find funny. I mean who would really think to redo Rihana's Umbrella song into a song/dance number about microorganisms called "Ellas." Or how about an anatomy number to Michael Jackson's "Thriller?" Or, a rendition of "Left my Heart in San Francisco?" about a heart surgery gone bad? Only we would do that and laugh at loud watching it.
The play was absolutely hilarious. Probably because, it's nerdy humor that only we would find funny. I mean who would really think to redo Rihana's Umbrella song into a song/dance number about microorganisms called "Ellas." Or how about an anatomy number to Michael Jackson's "Thriller?" Or, a rendition of "Left my Heart in San Francisco?" about a heart surgery gone bad? Only we would do that and laugh at loud watching it.
Tuesday, November 6, 2007
The Flash
 You know it's a good sign, when you get a flash--the first sign of red blood that oozes out of the butterfly tube. And then with a push of a tube, you have it, a nice flow of red warm blood that quickly drips to fill the tube.
You know it's a good sign, when you get a flash--the first sign of red blood that oozes out of the butterfly tube. And then with a push of a tube, you have it, a nice flow of red warm blood that quickly drips to fill the tube.Sunday, November 4, 2007
Daydreaming of Saturdays at Ocean Beach
 Everyday should be a day spent strolling the beach, camera in hand. My Saturday was unforgettable: me, my camera, and the great blue ocean.
Everyday should be a day spent strolling the beach, camera in hand. My Saturday was unforgettable: me, my camera, and the great blue ocean.It was actually warm enough to venture out to Ocean Beach, which is a short 20 minute Muni ride from my place. And for the first time since moving to SF, I finally spent some time in the Pacific Ocean. And the Ocean gave me a gift- sand in my sneakers that keeps resurfacing every time I go for a run or exercise.
Now it's time to prepare for another week of Cardio. Here's to a productive and relaxing week (with daydreaming about days spent on the beach).
Images: "Care-free" and "Easy-Going" (from my Collection taken at the Beach)
Friday, November 2, 2007
The Doctor Exam
 Who knew that saying "99" can be used to check for tactile fremitis?
Who knew that saying "99" can be used to check for tactile fremitis?Today we had another exam. This exam was a little different; it did not involve knowing facts and formulas and complex concepts. We were not sitting in a lecture hall. Instead, we were in a patient exam room. This test was unusual- it was the observed physical exam.
.JPG)




